Roux-en-Y Gastric Bypass

Basic Information
- Roux en Y Gastric Bypass is the most ‘tried and true’ bariatric operation
- It is particularly good for patients with Diabetes or Reflux (Heartburn)
- One Anastamosis Gastric bypass is a variation, but it is not good for patients with bad reflux
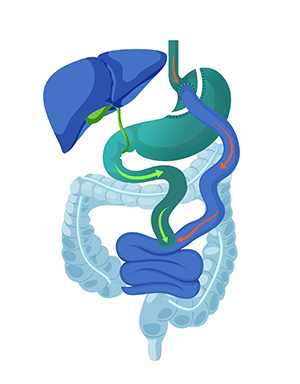
The stomach is divided to make a small upper “pouch”. The bowel is divided, one end joins the stomach, the other joins the bowel (intestine) lower down.
The food and the digestive juices are separated for around 2/5 the length of the small intestine.

Gastric Bypass Procedure
Gastric Bypass
Also known as a Roux Y or Roux en Y Bypass combines a small stomach pouch with approximately 2/5 of the small intestine bypassed. Food goes down one length of bowel and digestive juices the other until they meet. There is a join from the stomach to the intestine, and another from intestine to intestine.
Single Anastamosis Gastric Bypass
Also known as a One Anastamosis or ‘Mini’ Gastric Bypass bypass prevents the digestive juice from meeting the food for up to 2 meters, mixing with food just after the stomach. There is just one join and a ‘sleeve’ like pouch of stomach adds restriction. Single anastamosis bypass is much more common than Roux Y Bypass in Dr Crawford’s practice. Patients with significant reflux should have this only after significant consideration as the standard (Roux) bypass might be a better option.
The Surgery
Gastric Bypass is performed using laparoscopic (keyhole) techniques to staple off the stomach and create a diversion for the food to pass through some of the bowel without mixing with the digestive juices until lower down. This leads to some malabsorption which, along with the smaller stomach contributes to weight loss.
The surgery involves a number of small incisions in the abdomen and stapling of the upper stomach. The bowel is divided and one end joined to the stomach, the other is joined to side of the bowel lower down to make a ‘Y’ pattern.
The most important way weight loss occurs is through a substantial and prolonged decrease in appetite, brought on by powerful intestinal hormones that also work against type 2 diabetes. There is also a tendency to avoid carbohydrate rich foods because of an effect called ‘dumping syndrome’.
You will need to be on an ‘Ultra-low Calorie Diet’ before surgery. Optifast is taken for 2 weeks to replace ALL meals. If you feel have something else, then it needs to contain very few calories. (Salad or steamed vegetables without dressings or oil for a ‘treat’). Check with the nutritionist.
The usual stay in hospital is 3 post-operative nights.
Day 2-7: Fluids that could be sucked through a thin straw.
Day 7 to week 3-4: thick fluids progressing to puree.
Week 4+: Slow introduction of some more solid foodstuffs thereafter, as guided by the team.
Progress from thin to thick only after the thinner fluids are easily tolerated

Potential complications of Roux en Y Gastric Bypass
This is a complication that can occur early on. It is a failure of surgery or staples (rare) or a failure of healing. Leaks can occur at either join or on the staple line itself. Managing a leak can be difficult and you might need further procedures or even surgery to get it fully healed.
Bowel can become trapped under other bowel segments or due to scar tissue that can be severe and require urgent surgery.
This is an erosion that occurs near the stomach join that can cause bleeds, narrowing or perforation. It is a problem particularly in smokers. This is not a problem with Sleeve Gastrectomy.
This is usually experienced as Heart Burn. It is more an issue with Sleeve Gastrectomy and is a potential reason to opt for Roux Y Bypass instead.
A rare complication of weight-loss surgery is persistent nausea or vomiting. Further surgery could be required if there is a physical problem such as a narrowing that does not respond to endoscopic ballooning.
These include but are not limited to the following which are similar for almost any abdominal surgery.
-
Wound infection
-
Bleeding
-
Clots
-
Pneumonia
-
Heart trouble
-
Hernia
General Advice after Gastric Bypass
- Vomiting
- Vitamins
- Pregnancy
- Medication
- Nutritional issues and 'Dumping'
- Appointments
Vomiting
Patients may vomit or feel pain after food intake. This can be can be caused by swallowing too quickly, trapping air, or un-chewed chunks of food getting stuck. By eating slowly and calmly, you will learn to listen to the signals from your stomach. Notify Dr Crawford if new or persisting vomiting develops after you are home.
Vitamins
The bypass causes a reduction of absorption of some elements and vitamins. A chew-able or liquid vitamin mixture containing multivitamins, in particular the vitamin B complex, is recommended following surgery. Your nutritionist will give you advice around vitamins. You will need lab tests every few months to monitor your levels.
Pregnancy
The period between surgery and weight stabilisation is considered to be a period of starvation. It is not advisable to become pregnant during starvation, despite the fact that the foetus has priority over the mother with regard to food. Should you nevertheless get pregnant, it is advisable to let Dr Crawford and your nutritionist know. Wait 9-12 months before trying to become pregnant.
Medication
Tablets must be broken down into small pieces or crushed before they are taken. It is common that medication for conditions such as hypertension, diabetes or asthma may need to be altered (reduced) after the operation. You should consult your local doctor about this.
Nutritional issues and 'Dumping'
Patients after bypass may not absorb all their vitamins and minerals normally and usually require long-term supplements that will be overseen by a dietitian. Dumping syndrome is discomfort or dizziness associated with eating that can usually be managed by changing how you eat. Your nutritionist will give you advice should you require it.
Appointments
After surgery you must undergo regular check-ups as an outpatient. Initially, these check-ups will be carried out often, but will drop off quickly if everything is going ok.
Physical activity
It will be important to alter not only your eating habits, but also your level of physical activity. You should start exercising slowly after surgery. As weight loss is achieved, physical activities will gradually become easier.
Long-term follow up and lifestyle
In order to get the best results from your surgery, it is important that you are committed to long term changes. Regular consultations are necessary to review your progress, monitor your weight and health, advise you on diet and exercise and look for any long-term problems.
Your commitment to dietary and lifestyle changes is essential to ensure the success of your surgery. In the long term you should eat small healthy meals and drink only liquids containing little or no calories such as water, tea, coffee and sugarless drinks.
Regular exercise should be a part of your weight loss program and you should aim to exercise for at least 20 to 30 minutes every day.